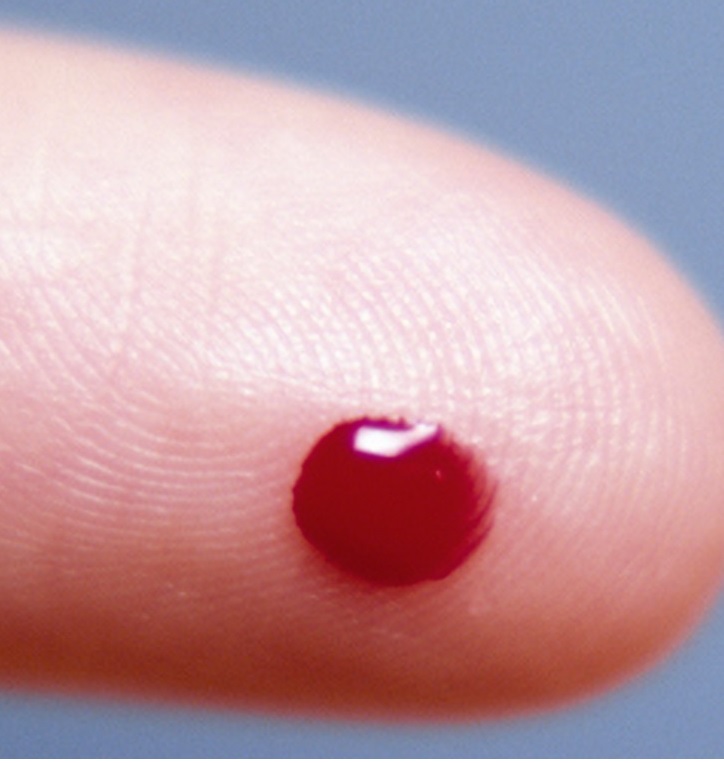
Bloodborne pathogens treatment
Universal precautions apply to which body fluids?
Cerebrospinal fluid
Blood
Semen
Vaginal secretions
Synovial fluid
Pleural and pericardial fluid
Amniotic fluid
In general, universal precautions do not apply to nasal secretions, feces, sweat, sputum, urine, vomitus, and tears unless they contain visible blood or have obvious signs of an infection.
Who requires training for bloodborne pathogens?
Any individual, irrespective of whether he or she is a healthcare worker, who is at risk for exposure to blood-borne pathogens needs to undergo training and pass the bloodborne pathogens test module. In general, the following professionals should undergo the bloodborne pathogens test:
- Healthcare workers including nurses, doctors, phlebotomists, lab technologists, etc
- First responders, EMTs, paramedics
- Fireman and law enforcement
- Researchers
- Medical laboratory personnel
- Nursing home staff
- Dentists and dental assistance
- Janitorial staff, housekeeping, cleaners
- Blood bank personnel
- School nurses, and all other school employees
- Funeral home employees including morticians
- Tattoo parlor personnel
This is not a complete list but in general, anyone who will come into contact with blood and body fluids should undergo the bloodborne pathogen module test.
Post-exposure treatment
Despite the best efforts and closely following safety precautions, accidental exposure to blood-borne pathogens does occur. Data show that doctors and nurses will suffer at least one needle stick at least once in their lifetime. And healthcare staff who work in the emergency room and operating theaters will suffer a needle or sharp injury one or more times in their career.
After exposure to a patient’s blood or body fluids, pathogens, the key is to act quickly. Every one in the workplace should follow the post-exposure protocol. OSHA requires that all employers offer FREE post-exposure and follow-up appointments to their employees who have been injured from a needlestick at no cost.
- After a needlestick or a sharp injury, the first thing to do is immediately wash the area with soap and water. If the blood or body fluid has involved the mucus membrane amounts of water or saline. Do this for at least 10-15 minutes
- After the initial cleaning, seek prompt medical attention either at the emergency department or the workplace occupational and health safety department
- According to the workplace policy, your injury should be documented and/or photographed.
Blood work
Depending on the severity of your needlestick injury and/or exposure to mucous membranes, your baseline blood work will be done to determine your hepatitis B, C, and HIV status. The blood work will also help determine if you have any protection against hepatitis B.
Treatment
Hepatitis B: If you have already been previously vaccinated against hepatitis B, no further treatment is required. However, if you have never received the hepatitis B vaccine or lack immunity to hepatitis B, you will be offered hepatitis B immune globulin and started on the hepatitis B vaccine.
Hepatitis C: There is no vaccine for hepatitis C but there are currently some very effective treatments to prevent the progression of hepatitis C and even obtain a cure. However, the treatment duration may vary from 1-6 months.
Tetanus: Although tetanus is not a blood-borne infection, you will be asked about your tetanus status if the injury has penetrated the skin. Tetanus vaccine is usually necessary for wounds from dirty objects or when the injury is deep. For only minor injuries, the recommendation is a booster if your tetanus shot was more than 10 years ago. If the wound is from a dirty needle or is a deep puncture wound, a booster is necessary if it has been more than 5 years since the last booster dose.
Post Exposure Prophylaxis (PEP) for HIV
The decision to prevent HIV infection will depend on the type of injury, severity, patient preference, and the HIV status of the source. In most cases, an infectious disease expert will be present to determine the need for treatment. In some cases, the consultant may start you on antiretroviral therapy and then discontinue it as more blood work data becomes available. But it is important not to delay post-exposure prophylaxis. Ideally, for HIV, post-exposure prophylaxis should start within 2 hours after exposure. Patients are normally have too take a 28-day course of antiretroviral medications.
Repeat blood test
Irrespective of the type of blood-borne organism suspected, repeat blood work is usually necessary because in some cases, some infections may show up late. For example, hepatitis B and C can take up to 3-6 months to show up in blood and HIV may take even longer. One must follow up with a healthcare provider for repeat testing until all the tests are negative.
Prevent infection transmission in the post-exposure period.
It is vital that you undertake precautions to prevent the spread of infections in the post-exposure period. This means that for the next 6 months, you will have to live life assuming you have an infection. During this window period, you should:
- Use a condom
- Practice safe sex
- Avoid getting pregnant
- Refrain from donating blood
- Avoid sharing personal care products with others like toothbrushes, razors, nail clippers, etc.
Follow the above precautions until your healthcare provider recommends that it is no longer necessary.