Weather Conditions and Sudden Cardiac Death: An In-Pulse CPR Special Report
Sudden cardiac death (SCD) is a devastating event, often striking without warning and leaving profound consequences for families and communities. It occurs when the heart suddenly stops beating effectively, leading to a rapid loss of consciousness and, if not treated promptly, death.
While numerous factors contribute to the risk of SCD, including underlying heart conditions, genetic predispositions, and lifestyle choices, research has increasingly pointed to the role of environmental factors, particularly weather conditions, in influencing the occurrence of these tragic events.
This content explores the various weather conditions that are most often associated with an increased risk of sudden cardiac death, delving into the underlying mechanisms and epidemiological evidence that support these connections.
Introduction to Sudden Cardiac Death
Sudden cardiac death is defined as an unexpected death caused by cardiac arrest in a person with or without pre-existing heart disease. It typically results from a malfunction in the heart’s electrical system, leading to a chaotic rhythm called ventricular fibrillation, which prevents the heart from pumping blood effectively.
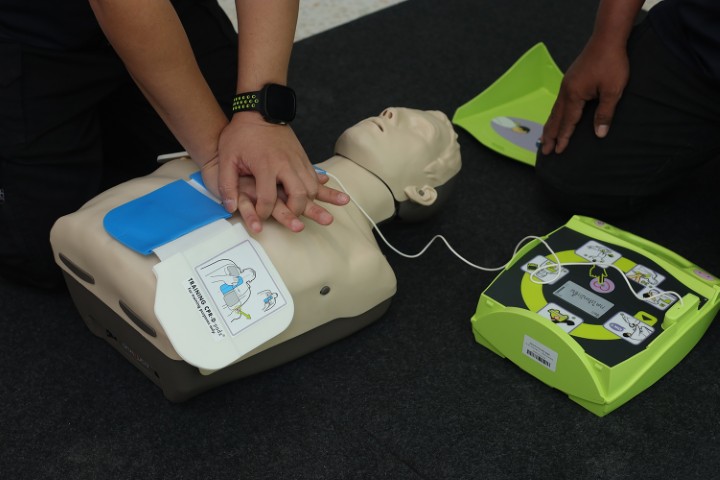
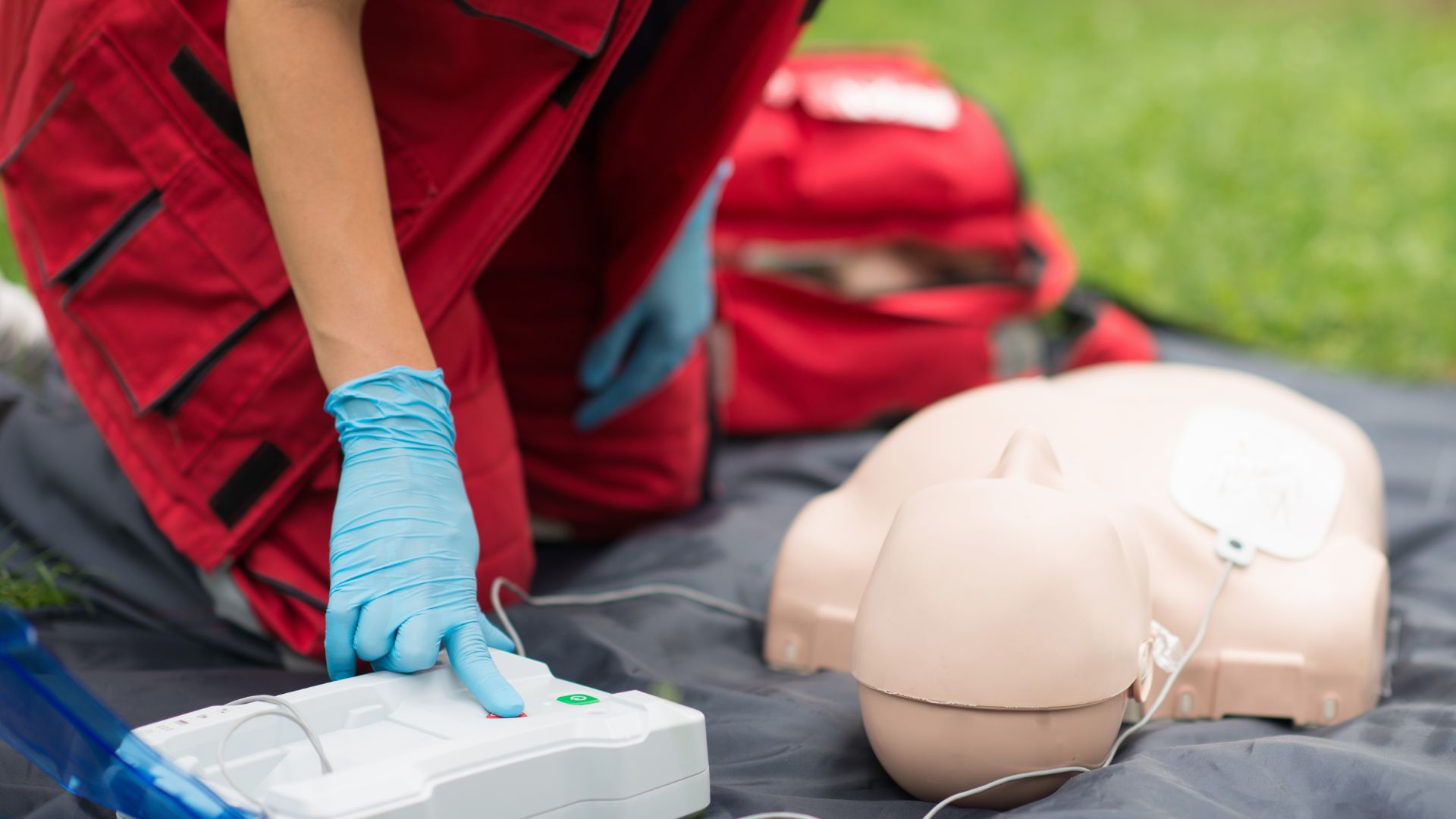
Without prompt intervention, such as cardiopulmonary resuscitation (CPR) and defibrillation, death occurs within minutes. While SCD can affect individuals of all ages, it is more common in adults, particularly those with underlying heart disease.
Many factors contribute to the risk of SCD, including coronary artery disease, heart valve problems, cardiomyopathy (disease of the heart muscle), and congenital heart defects. Lifestyle factors such as smoking, a sedentary lifestyle, and a poor diet also play a role. However, beyond these individual risk factors, external environmental conditions can also exert a significant influence.
The Influence of Weather Conditions
Weather conditions encompass a wide range of atmospheric phenomena, including temperature, humidity, air pressure, wind speed, and precipitation. These factors can fluctuate significantly throughout the day and across different seasons, exerting varying degrees of stress on the human body. For individuals with underlying heart conditions, these stresses can be particularly challenging, potentially triggering events that lead to SCD.
Temperature Extremes
One of the most well-studied aspects of weather’s influence on cardiac events is the impact of temperature extremes. Both extreme heat and extreme cold have been linked to an increased risk of SCD.
Heat Waves: During periods of extreme heat, the body works harder to maintain its core temperature. This involves increased heart rate, dilation of blood vessels, and sweating, which can lead to dehydration and electrolyte imbalances.
These physiological stresses can place additional strain on the heart, particularly in individuals with pre-existing cardiovascular disease. Several studies have shown a clear association between heat waves and increased rates of cardiac events, including SCD.
Cold Spells: Similarly, extreme cold can also be a trigger for SCD. Exposure to cold leads to constriction of blood vessels, which increases blood pressure and the workload on the heart. The body also shivers in an attempt to generate heat, further increasing metabolic demands. Cold temperatures have been shown to increase the risk of angina (chest pain), heart attacks, and arrhythmias, all of which can precipitate SCD.
Air Pollution
Air pollution is another environmental factor that has been increasingly linked to cardiovascular events, including SCD. Pollutants such as particulate matter (PM), nitrogen dioxide (NO2), and ozone (O3) can have detrimental effects on the cardiovascular system. Inhalation of these pollutants can trigger inflammation, oxidative stress, and changes in blood clotting, all of which can increase the risk of heart attack and arrhythmias.
Particulate Matter: Particulate matter, especially fine particles (PM2.5), can penetrate deep into the lungs and enter the bloodstream, where they can trigger systemic inflammation and contribute to the formation of blood clots. Studies have consistently shown a link between elevated levels of PM2.5 and increased rates of cardiovascular mortality, including SCD.
Other Pollutants: Nitrogen dioxide and ozone are also associated with adverse cardiovascular effects. NO2, primarily from vehicle emissions, has been linked to increased risk of heart attacks and arrhythmias. Ozone, a component of smog, can cause inflammation and oxidative stress in the lungs and cardiovascular system.
Atmospheric Pressure
Changes in atmospheric pressure, particularly sudden drops associated with storms, have also been suggested as potential triggers for cardiac events. While the evidence is not as robust as for temperature and air pollution, some studies have indicated a possible association between low atmospheric pressure and increased risk of SCD.
The mechanisms underlying this association are not fully understood, but it is thought that changes in pressure may affect blood viscosity and heart rate.
Wind Speed and Precipitation
Wind speed and precipitation can also indirectly influence the risk of SCD. High winds can exacerbate the effects of temperature extremes, making cold weather feel even colder and hot weather feel more oppressive.
Strong winds can also contribute to the dispersion of air pollutants, potentially increasing exposure. Precipitation, particularly heavy rain or snow, can also add to the physical stress on the body, especially for individuals with underlying health conditions.
Seasonal Variations
Considering these individual weather factors collectively, there are clear seasonal variations in the occurrence of SCD. Rates tend to be higher in the winter months, particularly during periods of cold weather and increased respiratory infections, and also elevated during summer heat waves. These seasonal patterns highlight the complex interplay between multiple weather factors and their impact on cardiovascular health.
Underlying Mechanisms
Several mechanisms have been proposed to explain how weather conditions can trigger SCD. These include:
- Increased Myocardial Oxygen Demand: Both heat and cold stress increase the heart’s workload and oxygen demand. This can be particularly problematic for individuals with coronary artery disease, where blood flow to the heart is already compromised.
- Electrolyte Imbalances: Excessive sweating during heat waves can lead to dehydration and electrolyte imbalances, which can disrupt the heart’s electrical system and trigger arrhythmias.
- Blood Viscosity Changes: Cold weather can increase blood viscosity (thickness), making it harder for the heart to pump and increasing the risk of clot formation.
- Inflammation and Oxidative Stress: Air pollution and other environmental stressors can trigger inflammation and oxidative stress, which can damage the heart and blood vessels and increase the risk of arrhythmias and blood clots.
- Autonomic Nervous System Activation: Both physical and emotional stress associated with extreme weather can activate the autonomic nervous system, leading to changes in heart rate and blood pressure.
Epidemiological Evidence
Numerous epidemiological studies have explored the relationship between weather conditions and SCD. These studies have used a variety of methods, including time-series analysis, case-control studies, and cohort studies, to examine the association between specific weather parameters and the occurrence of cardiac events.
| Study Aspect | Description |
| Time-Series Analysis | Examines trends over time to correlate weather patterns with SCD rates. |
| Case-Control Studies | Compare individuals who experienced SCD with control groups to identify weather-related risk factors. |
| Cohort Studies | Follow groups of individuals over time to assess how weather exposure affects their risk of SCD. |
Findings from these studies have consistently shown a clear link between temperature extremes, air pollution, and increased risk of SCD. The strength of these associations varies depending on the specific population, geographical location, and study methodology, but the overall consensus supports the notion that weather conditions play a significant role in triggering cardiac events.
Vulnerable Populations
Certain populations are more vulnerable to the effects of weather extremes and air pollution on cardiovascular health. These include:
- Older adults: Aging is associated with a decline in physiological function and increased susceptibility to temperature extremes.
- Individuals with pre-existing cardiovascular disease: These individuals already have compromised heart function and are more likely to be affected by additional stress.
- People with respiratory conditions: Conditions such as asthma and chronic obstructive pulmonary disease (COPD) can be exacerbated by air pollution and temperature extremes.
- Low socioeconomic status groups: These groups may have limited access to resources such as air conditioning or heating, making them more vulnerable to weather extremes.
Preventive Measures
Given the evidence linking weather conditions to SCD, several preventive measures can be taken to reduce risk. These include:
- Staying Informed: Monitor weather forecasts and air quality reports, and take precautions during extreme weather events.
- Hydration: Drink plenty of fluids, especially during hot weather, to prevent dehydration and electrolyte imbalances.
- Appropriate Clothing: Dress appropriately for the weather, wearing layers in cold weather and lightweight, breathable clothing in hot weather.
- Avoiding Exposure: Limit outdoor activity during extreme weather and high air pollution days.
- Medication Management: Ensure that prescribed medications are taken as directed, and consult with a healthcare provider about potential weather-related adjustments.
- Air Purifiers: Use air purifiers indoors to reduce exposure to air pollution.
- Community Support: Check in on elderly neighbors or family members during extreme weather events.
Conclusion
Weather conditions play a significant role in influencing the risk of sudden cardiac death. Temperature extremes, air pollution, and other atmospheric factors can place considerable stress on the cardiovascular system, particularly in individuals with pre-existing heart disease.
By understanding the mechanisms underlying these associations and taking preventive measures, it is possible to reduce the risk of weather-related cardiac events and protect vulnerable populations.
Further research is needed to fully elucidate the complex interplay between weather, environmental factors, and cardiovascular health, and to develop more effective strategies for prevention and intervention.