Cape Coral Hospital CPR classes
Cape Coral Hospital staff welcome to attend CPR classes with In-Pulse CPR
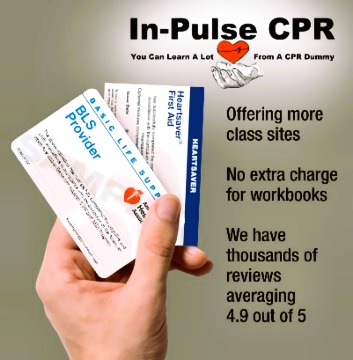
Our classes provide you with the necessary CPR certification (American Heart Association for Healthcare Providers) for job requirements with Cape Coral Hospital Ft Myers FL.
Per hospital guidelines: …providing documentation of a current CPR certification.. is required. An American Heart Assoc BLS certification is the national standard for medical students.
Please be assured that all nursing or healthcare employment in the area will accept our program to fulfill your CPR requirements. When signing up please select a BLS Provider course.
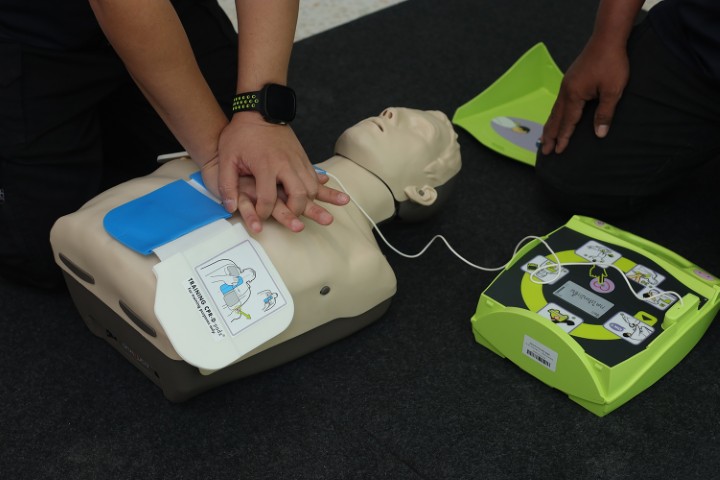
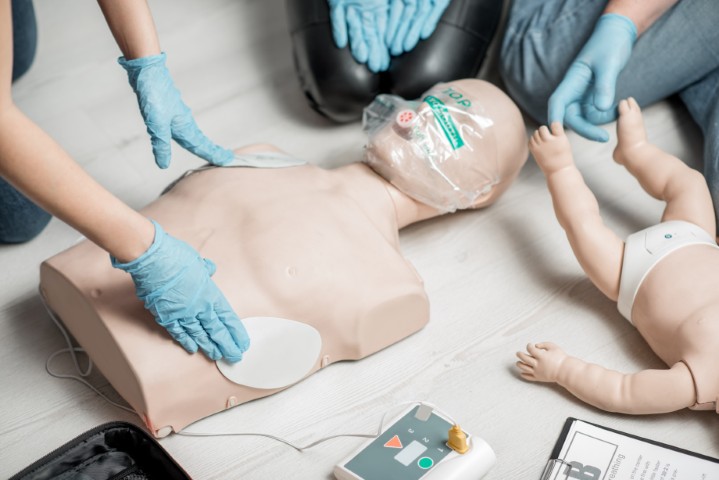
At In-Pulse CPR we take pride in our quality of teaching. We use the latest technology and state-of-the-art equipment to provide for an interactive, experiential learning environment. We make sure that each student leaves the classroom feeling confident in the skills they gained. Our classes are fun too!
We offer CPR certification at multiple locations in the area
Click here to View our Class Calendar
We offer the following certifications:
BLS Healthcare CPR / Heath care Professional – This is the certification Cape Coral Hospital healthcare employment requirements would need to register for. These classes are showing in yellow on our calendar.
Heartsaver CPR
Heartsaver AED
Heartsaver First Aid
and More…
Cape Coral Hospital health care